Universal T-Cell Therapy
Universal T-cell therapies
If you have been reading our articles for a while, or generally keep up with cancer therapeutics in the news you must have heard of T-cell therapy. A big problem with current T-cell therapies is that they target a very specific marker of cancerous cells and so, when a mutation results in the cancer cells no longer expressing that marker, the cancer will relapse and evade the therapy. To address this problem, a group at the University of Pittsburgh developed a new approach wherein they had an antibody that can target a specific marker bound to a molecule called ‘BG’, which can be found by CAR-T or SynNotch-T cells, mediate the expression of a protein called ‘SNAPtag’ to kill the cancer.
That suddenly became a lot of jargon so let’s break some of it down. First, CAR-T cells are cells expressing the chimeric antigen receptor (CAR), an artificially modified receptor that gives T-cell the ability to kill other cells expressing the target protein. SynNotch-T cells work in a similar way but work by inducing or restricting the expression of a gene. So if a SynNotch T-cell finds its target, it will induce the expression of another protein, say CAR to kill the target cell. The SNAPtag approach adds more flexibility to these therapies. With current approaches, if cancers stop expressing the protein that the therapy targets, a new therapy with a different target has to be used. This requires the designing of a new cell to put into a patients body which requires more time, more money, and introduces new unknown factors. In the case of the SNAPtag approach, if the cancer stops expressing the initial target, a new antibody against a new target can be created and linked to BG which can be put in the patients allowing the SNAPtag T-cells to target the cancer again.
This will allow using the same set of modified T-cells to target multiple targets and treat cancer as it mutates. This may also help save costs related to engineering new T-cells every time the cancer mutates. Typically CAR-T cell therapy costs several hundred thousand dollars, if the same set of T-cells can be reused with new targets, it will help greatly reduce the cost of treating cancer using T-cell therapies.
Overall, this is a very good advancement and can potentially help treat cancer far more effectively while simultaneously making these treatments more accessible. Although like all technology we discuss in this newsletter, it still needs more testing.
Read the full paper:
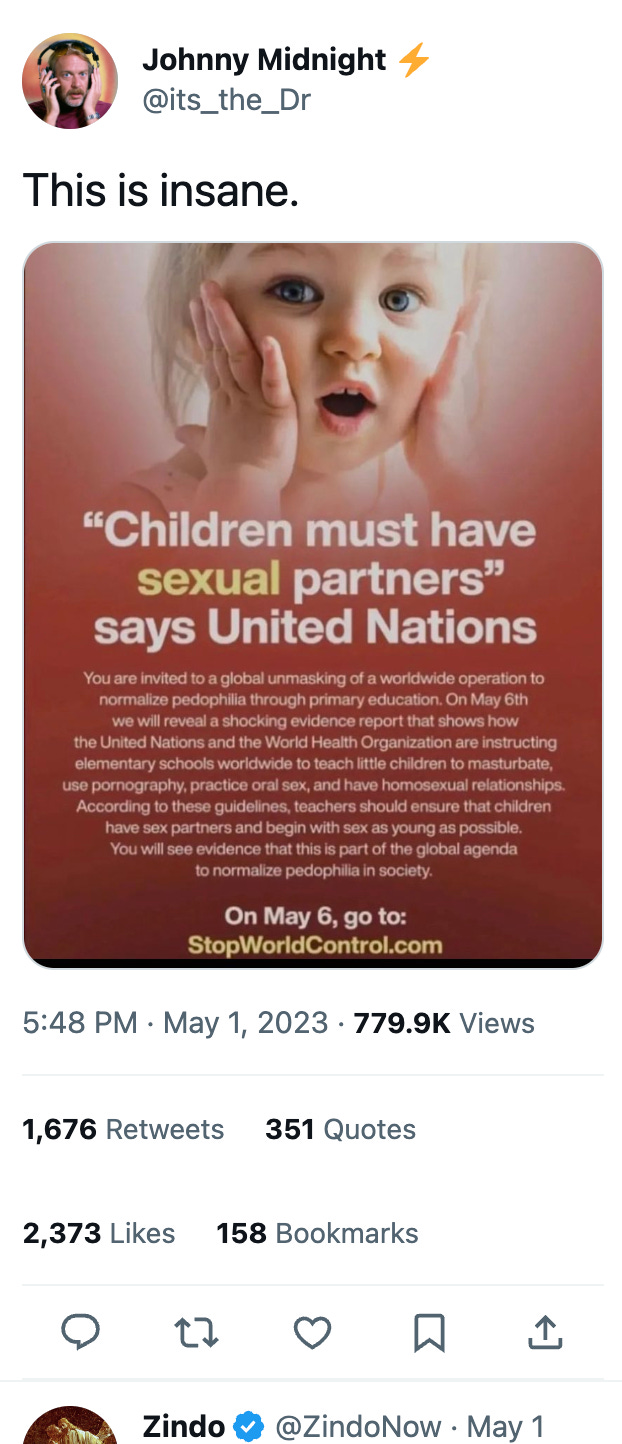
Featured Fake News
Yeah, this is fake.
The claim originates from a typical fake news website which has grossly misinterpreted an actual UN report calling for age-appropriate sex education.
As we’ve discussed before, age-appropriate sex education is a progressive policy and it can most easily be seen in action in the Netherlands where applying such a system to public education strongly correlated with a decrease in teen pregnancies, more responsible and safer sexual practices, and most people finding their first sexual partners at an older age. This is very different from the abstinence focused sexual education in the United States.
Make no mistake, here at Unmasking Medicine we are not advocating for it to be imposed everywhere as there are very real challenges. We are just saying that the above claim is false.
If you are enjoying the Unmasking Medicine Newsletter, why not share it? You can get 3 free stickers for every 3 people who subscribe using this form!